Harvard faculty members discuss state of research
Observing disease growth is a major boon of stem cell research
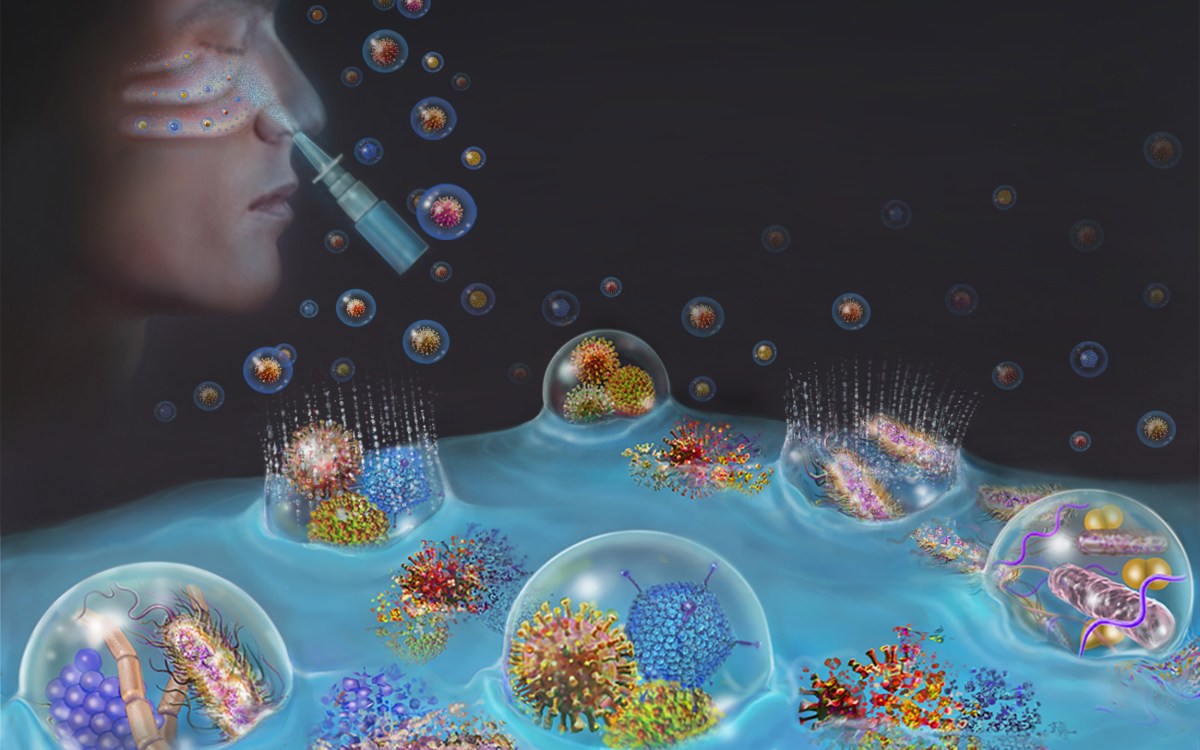
A panel of experts said Tuesday (March 11) that stem cell research’s biggest impact on patients’ health likely won’t come from therapies that inject stem cells or implant tissues made from them, but rather from the knowledge gained by examining diseased tissues grown from the cells.
Kenneth Chien, Charles Addison and Elizabeth Ann Sanders Professor of Basic Science at Harvard Medical School, head of the Harvard Stem Cell Institute’s Cardiovascular Program, and director of Massachusetts General Hospital’s Cardiovascular Research Center, said he expected stem cell research to transform our understanding of diseases over the next 10 years or so and lead to new drugs and treatment strategies.
Stem cells’ impact on that transformation will come as scientists study diseased tissues grown from the cells of people afflicted by particular ailments. By growing cells themselves, they can watch as a disease progresses and better understand the driving forces behind it.
Chien was less optimistic about stem cells’ impact on the future of cell replacement therapy — growing new cells, tissues, and even organs from stem cells to replace a patient’s diseased ones. For some ailments, he said, implanting replacement tissues grown from stem cells may turn out to be the best approach. But he also said stem cell-based therapy comes with its own complications — like the danger of an implanted cell turning cancerous — and he doesn’t see such therapy ever completely replacing pharmaceuticals and other traditional approaches.
Chien made his comments during a public forum sponsored by the Harvard Stem Cell Institute Tuesday evening at the Fairchild Biochemistry Building. The event, attended by about 80 people, was the third in the institute’s public forums this year, which aim to stimulate discussion of the many aspects of stem cell research, such as science, health care, ethics, and government policy.
The event, “Stem Cells and Key Diseases,” was moderated by Assistant Professor of Molecular and Cellular Biology Kevin Eggan and featured experts in three different areas of stem cell science: diabetes, neurology, and cardiology. Joining Chien were Professor of Medicine Gordon Weir, head of the Harvard Stem Cell Institute’s Diabetes Program and head of the Joslin Diabetes Center’s Section on Islet Transplantation and Cell Biology; and Professor of Surgery and of Neurology Jeffrey Macklis, head of the Harvard Stem Cell Institute’s Nervous System Program and director of Massachusetts General Hospital’s Center for Nervous System Repair.
Weir kicked the event off, discussing goals and progress in diabetes-focused stem cell research. The goal in such work is, he said, simple: to increase the number of insulin-producing cells. There are two main thrusts for research — one focuses on creating new cells for implantation, and the second focuses on getting the remaining cells in the pancreas to multiply.
“All we want to do is replicate insulin-producing islet cells,” Weir said. “In the end, the cause of diabetes is not enough [insulin-producing] cells.”
Though the goal is simple, achieving it is not. Diabetes is an autoimmune disease, where the body for some reason destroys its own cells, which complicates transplanting cells made from a person’s own tissues. Research aimed at creating new insulin-producing cells is focused on understanding the developmental steps a cell goes through to develop from a stem cell to an insulin-producing beta cell.
Considerable progress has been made on this front already. In February, researchers reported that they implanted cells into mice that are precursors to beta cells. The cells went on to develop into mature beta cells. The problem, the researchers reported, is that some of the cells also became cancerous, which has to be addressed before such therapy is used in people.
Macklis gave the audience a view of the complexity of the nervous system, saying its diversity presents a hurdle to any work on regenerative medicine. There are hundreds, if not thousands, of types of different neurons in the brain, he said. They function as differently as a family sedan and a jet plane. Some of the research today focuses on understanding the specific types of neurons that are attacked in Amyotrophic Lateral Sclerosis (ALS), or Lou Gehrig’s disease, so they can try to prevent the death of those cells, support diseased ones, and enhance regeneration.
Chien drew an analogy between today’s stem cell research and heart transplantation surgery in the past, saying it took 20 years for researchers and clinicians to get it right. We’re at the beginning of a similar process with stem cells, he said, but the scientific work will eventually lead somewhere.
“We have to be careful about not raising false hopes,” Chien said. “We have to let science take us there.”