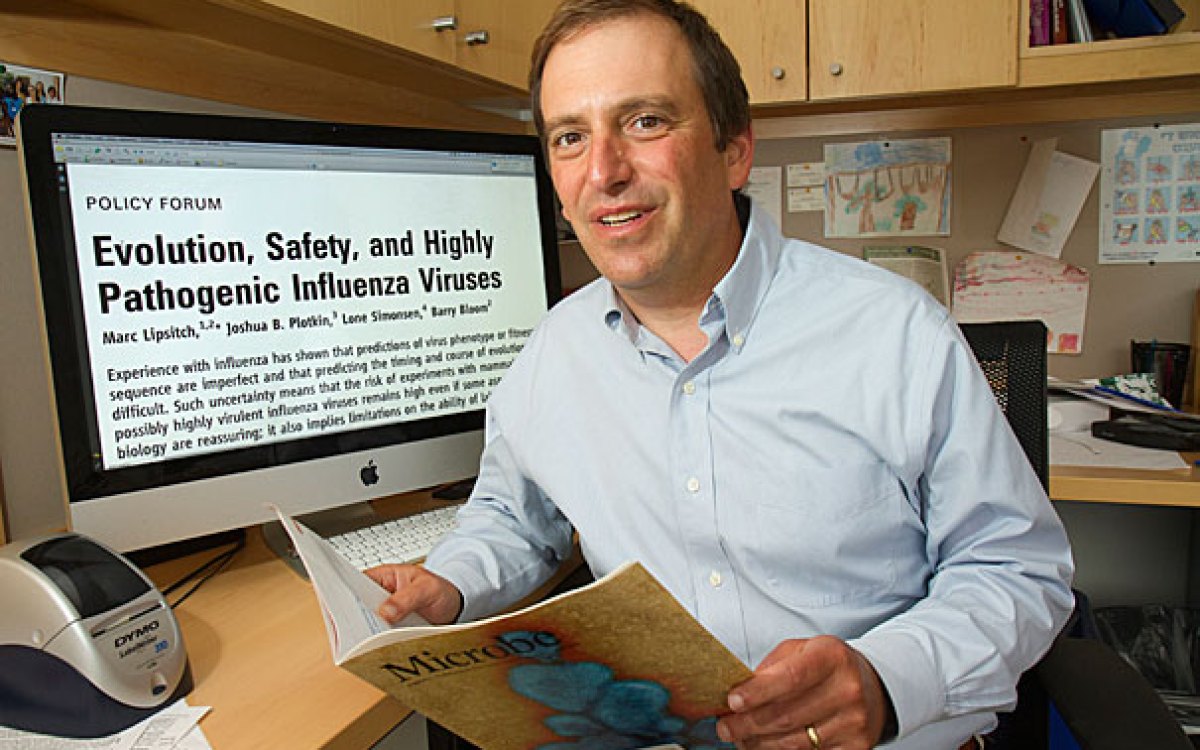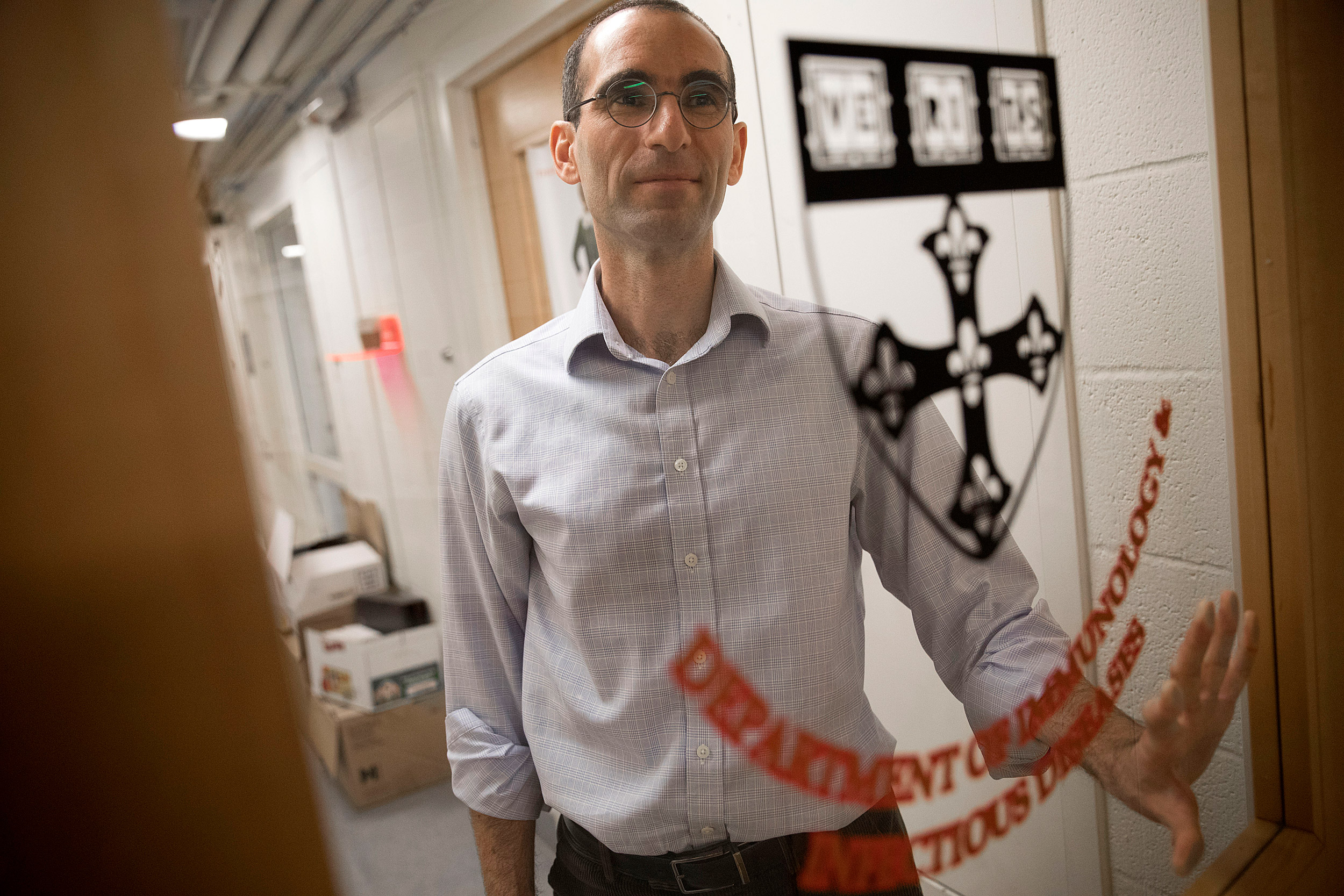
Assistant Professor of Immunology and Infectious Diseases Yonatan Grad talks about why this year’s seasonal flu has been so severe and why it is so important for eligible patients to get vaccinated.
Kris Snibbe/Harvard Staff Photographer
Everywhere you look, flu
Better late than never on vaccination, expert says
Yonatan Grad, an assistant professor of immunology and infectious disease at the Harvard T.H. Chan School of Public Health, has seen up close what the Centers for Disease Control and Prevention confirms: We are in the middle of a nasty flu season. A flu shot still makes sense, Grad noted, even if the results don’t match the effectiveness of vaccination against other ailments. “A vaccine doesn’t have to be perfect to be helpful,” he said. “It is better to have some benefit than none.”
Q&A
Yonatan Grad
GAZETTE: How does this flu season stack up?
GRAD: It is a bad season but it’s a bad season on par with what we expect from the type of flu that is circulating. There are two main types of influenza that infect humans and cause disease: influenza A and influenza B, and within A there are subtypes H3N2 and H1N1, and then there are a couple of strains of B, all of which co-circulate. In a flu season, either H3N2 or H1N1 viruses dominate. The H3N2 seasons tend to be more severe, both in terms of the number of people who get infected and the severity of infection. And we are in an H3N2 year. Recent H3N2 years, like 2012‒2013 or 2014‒2015, have pretty similar numbers.
GAZETTE: How well did this year’s vaccine match up with the composition of the viruses that are out there?
GRAD: There’s been a lot of interest because there was an interim estimate from the season in Australia that suggested that the vaccine effectiveness there for the H3 component was around 10 percent. That seems particularly poor, though in most years the H3 component has a vaccine effectiveness of only around 40 percent.
We don’t yet know what the case is in the U.S. It’s not clear if the same population of viruses is also here, so we are waiting to see what the vaccine effectiveness is in North America.
The flu vaccine is intended to protect you in several ways: by reducing your likelihood of getting infected, by reducing the symptoms — the severity of disease — if you get infected, and by reducing the extent to which you are infectious. So it has many different potential benefits. Even though the vaccine effectiveness is not as high as what we see with, say, measles — which has a vaccine effectiveness of 95 to 98 percent — there is still a benefit. A vaccine doesn’t have to be perfect to be helpful — it is better to have some benefit than none.
GAZETTE: According to the Centers for Disease Control and Prevention, the U.S. vaccination rate is under 50 percent. Would the shot be more effective if more people got it?
GRAD: We think so. The idea is that you would have an increase in “herd immunity.” The more people are protected, the less likely it is that the influenza will spread in a population. So a higher uptake of the vaccine protects not only the people who are vaccinated, but also people around them who haven’t gotten the vaccine or who can’t get the vaccine for some reason.
GAZETTE: Should everyone get a flu shot?
GRAD: It’s recommended that everyone 6 months or older who does not have contraindications should get vaccinated.
GAZETTE: Why is it not as effective as the measles and chicken pox vaccines, in which you get your shot and your booster and you’re done? Is it because the virus mutates quite a bit, so it’s never exactly the same virus?
GRAD: That’s one of the traditional explanations and one that certainly seems to be the case, as the flu evolves from season to season. What you’re trying to do is immunize against an evolving population of viruses. But it’s also the case that people may not develop responses against the right part of the vaccine virus and so the response that you generate may not effectively protect against what’s circulating. It may also be that the different strains that we use in the vaccine vary in their ability to elicit a protective immune response. So we think there are different components to why the vaccine may not work.
GAZETTE: Is this something that we can improve on or are we stuck with this because the flu virus mutates so much and the different strains create a complex flu landscape?
GRAD: We’re not stuck with it. It’s an active area of research and people are working toward a universal influenza vaccine. The idea is that it’ll take the guesswork out of predicting which influenza strains will circulate each year and thus protect us against multiple different flu strains. There is currently a universal flu vaccine in clinical trials and a number of companies are working on other types of universal influenza vaccine.
GAZETTE: Any predictions for the rest of this season? It seems like it’s fairly early. Should folks be on their guard?
GRAD: I think there’s the classic line, “It’s very hard to make predictions, particularly about the future.” That said, most models predict that the season will peak this month. An important point is that it’s not too late to get a flu vaccine — the influenza season will likely continue for another few months.
GAZETTE: If you’ve gotten the flu already this season, are you safe or can you potentially get it again?
GRAD: Since multiple types of flu are circulating and causing disease, even if you’ve been infected with one type of influenza, you could still benefit from a vaccine to protect against infection by the others. And unless you’ve been tested, you probably don’t know for sure whether you’ve had the flu.