Having kids exercise an hour each day before school has been shown to lower BMI and encourage academic engagement according to a study by postdoctoral student Rachel Whooten.
Rose Lincoln/Harvard Staff Photographer
Giving kids a running start
MGH researchers measure impact of before-school exercise program on emotional, physical health
A before-school physical activity initiative started by a group of moms is an effective path to helping kids lose weight, according to a study by researchers from Massachusetts General Hospital for Children and Harvard Medical School.
The K-8 BOKS program, which has spread to 2,700 schools in four countries and attracted sponsorship from sneaker giant Reebok, requires little from school districts by way of staff and equipment, relying on volunteer leaders and emphasizing simple, accessible activities.
Rachel Whooten, a postdoctoral fellow in pediatric endocrinology, worked on the study with Professor of Pediatrics Elsie Taveras, project manager Meghan Perkins, and analyst Monica Gerber. We asked Whooten about the findings.
Q&A
Rachel Whooten
GAZETTE: What’s the state of exercise in schools today? Are kids getting the recommended amount through gym class?
WHOOTEN: When kids are being active, most of it is happening in the schools. But the unfortunate thing is the time that kids are actually being active in schools is not enough.
The official recommendation is for 60 minutes a day of physical activity, and only about 50 percent of kids have physical education offered even weekly. There are opportunities for recess in some schools, but the majority of kids aren’t getting enough physical activity. A lot of that is due to an increasing emphasis on academics, and also the reality that it’s difficult to find the resources to support physical activity in schools.
GAZETTE: Your study examined an exercise program called Build Our Kids’ Success. Could you describe it?
WHOOTEN: It’s a program based on the idea of fitting physical activity in before school. It was started by a group of moms outside of Boston who realized, as they were waiting for the bus with their kids, the kids just naturally wanted to run around.
So the moms started a physical activity program for their kids and were able to turn that into a much broader movement, which is now BOKS. It has been catching on in schools throughout Massachusetts as well as throughout the country and internationally. Basically, kids come before school and are led by a group of volunteers — who can be parents, or teachers, or nurses, and who attend a short training and then have resources for a curriculum available online. Kids are active for about an hour.
GAZETTE: What did you do and what did you find?
WHOOTEN: Three communities outside Boston had independently decided to start the BOKS program and chose whether to do it two days a week or three days a week, based on the resources in their schools. We compared kids who were in the two-days-a-week program, the three-days-a-week program, and those who did not participate.
One key thing to know is that it was not a randomized controlled trial. In partnership with the schools, any kid who wanted to participate in the BOKS program was able to participate in the BOKS program. So there is potential that there are differences between the kids who chose to participate and those who chose to not participate. That’s a limitation of the research.
There was a pretty large sample size — we had about 700 kids from kindergarten to eighth grade who were participating in the study. The BOKS program occurs over 12 weeks, so we had baseline and 12-week follow-up measures of height and weight. All kids over 8 years of age completed surveys on social and emotional functioning. The surveys [measured] how engaged they are in the school, positive feelings, how much energy they have, how relationships with friends are going, and their life satisfaction.
We found a favorable change in the body mass index in kids participating in the program three days a week compared to those who weren’t participating at all. We also found different results between the two-days and three-days-a-week groups for social-emotional wellness outcomes. The two-days-a-week group had improvements in positive feelings and vitality/energy, while the three-days-a-week group had improvements in student engagement.
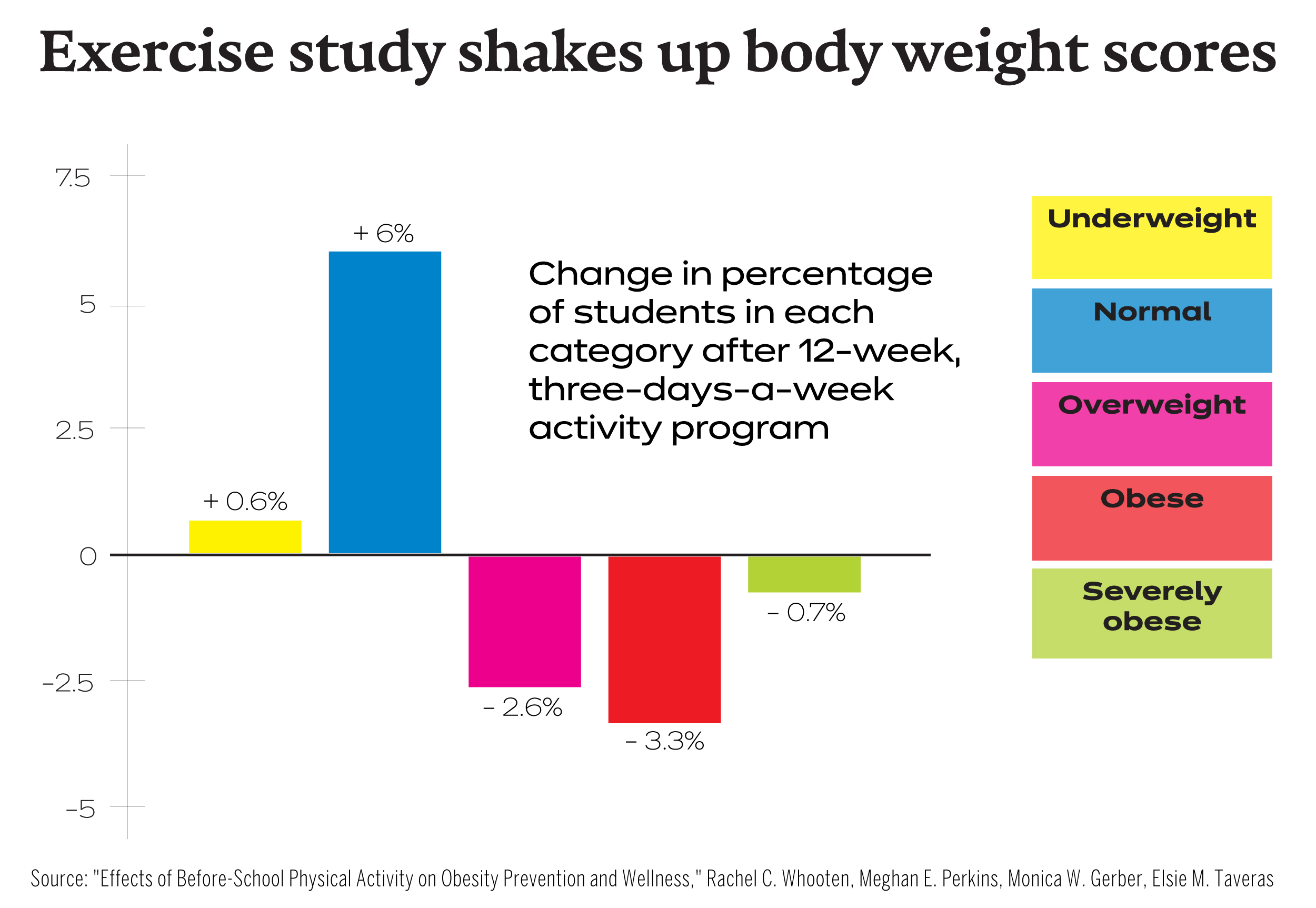
Graphic by Rebecca Coleman/Harvard Staff
GAZETTE: As far as BMI, does it mean that if you do this program, it should be three days a week?
WHOOTEN: The results do bring up the question of what the intensity of the program should be.
The U.S. Preventive Services Task Force — looking at a much broader range of physical-activity interventions in kids — found that in order for a program to be effective you had to have over 27 contact hours over a two- to three-month period. The two-day-a-week program falls below that amount of contact time while the three-day-a-week program falls above that contact time. So the findings in the three-days-a-week group of our study do fall within those guidelines, as far as the doses of physical activity needed in order to achieve BMI differences.
GAZETTE: Is it safe to say then, that if you do the three-day-a-week program, that the kids are more likely to lose weight and be better engaged in school? Is that the takeaway?
WHOOTEN: I would say that. I think one thing too, though, is that for obesity prevention, we’re looking at weight maintenance as opposed to weight loss. So finding a decrease in BMI, that’s great. But we also found that compared to baseline measures, more kids were in the healthy-weight category in the follow-up in the three-days-a-week group versus the two-days-a-week group and control.
GAZETTE: How important is it that the program occurs before school?
WHOOTEN: A lot of time, when we try to make kids more physically active in school, it takes time away from academics or takes resources from other things at the school. After school is a time when some kids are already involved in programs and this wasn’t a study of whether it’s better to participate in soccer or dance or walking or playing outside, for example. The before-school time avoids this issue of potential unintended consequences of physical activity during or after school.
In the before-school time period, there is less competition — if kids are doing anything, it may be something sedentary, like watching TV, playing on an iPad. The program takes this time when kids normally might not be doing anything and adds some positive behavior in. And elementary school starts a little bit later, so for a lot of parents it’s a situation where the program gives them a place to take kids in the morning and have them do healthy behaviors.
GAZETTE: How does this fit in with childhood obesity? Have there been any signs of the obesity epidemic in children declining or plateauing?
WHOOTEN: A couple of years ago, there did seem to be research supporting a decrease in obesity in the younger age groups. Unfortunately, in recent weeks more updated data came out that obesity rates are still increasing, so maybe the bright spots we thought we saw weren’t actually there. So we’re going back to the drawing board and seeing what interventions are out there and what we can do to be successful.